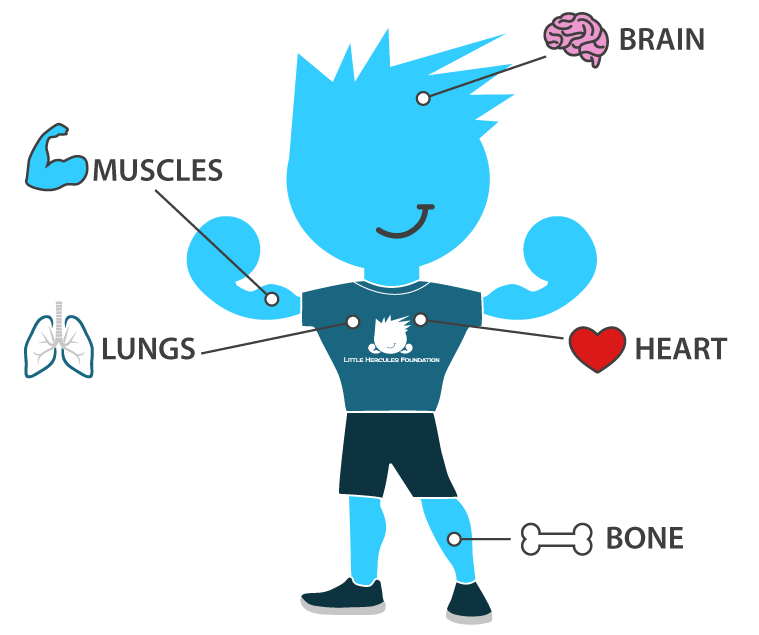
Muscles
Loss of muscle strength and function is progressive in Duchenne patients. Dystrophin helps maintain and heal muscle after normal use. With little to no dystrophin production, Duchenne muscles are damaged and replaced by connective tissue and fat. Early on, common motor skills are delayed, followed by slow weakening of the core skeletal muscle in early childhood. This loss of muscle strength spreads to the lower and upper limbs in adolescence, taking away the ability to walk and to perform essential daily living tasks independently such as dressing, eating, and bathing.
Bone
Duchenne patients typically have weakened bones and low levels of Vitamin D at onset. Steroids, commonly prescribed to address the skeletal muscle impacts, contribute to poor bone health by decreasing the calcium levels in bones. Over time, bones thin and become more brittle, leading to serious bone health issues, such as osteoporosis. This makes those living with Duchenne at high risk for fractures and breaks, which can have devastating impacts. With weakened skeletal muscles in the back, Duchenne patients are susceptible to scoliosis and compression fractures, often requiring serious, corrective surgery. Lastly, joints in feet, knees, elbows, etc. can become locked in one position as loss of ambulation occurs.
Brain
A small amount of dystrophin exists in the brain. Without it, people living with Duchenne are more likely to have development delays in learning, behavior, and social/emotional health compared to their peers. Specifically, this can lead to weakness is executive function skills, such controlling impulses and emotions, flexible thinking, and working memory, and trouble with friends or in a school/learning environment. For patients and caregivers, this can often feel like the most complex and troubling impact to manage among Duchenne patients. Not only is the spectrum of psychosocial health so vast, but ensuring overall well-being and self-image is important as patients adjust to the stages of Duchenne and seek support from those around them.
Heart
Your heart is a muscle too. The lack of a sufficient amount of dystrophin leads to weakening and scarring of the heart muscle. Although progression varies, heart disease will eventually affect all those living with Duchenne. The heart’s ability to pump blood properly throughout the body is impacted. Changes to heart rate and/or rhythm can also occur as patients with Duchenne get older. Damage to the heart, otherwise known as cardiomyopathy, begins in early stage before symptoms even appear. Cardiomyopathy and heart failure are the leading cause of death in Duchenne patients.
Lungs
Weakening of those muscles around the lungs that are critical to breathing, including the diaphragm, makes it difficult for those living with Duchenne to breathe and cough. Duchenne patients eventually breathe at an abnormally slower rate, increasing the amount of carbon dioxide in the blood. Breathing and coughing typically start to become problematic after the loss of ambulation occurs between the ages of 8-12. Patients may need to begin to use a breathing assist machine at night as teenagers, progressing into full time breathing assist or ventilation machines as young adults.